Biologic medications that neutralize IgE antibodies have long been considered a promising food allergy treatment. Now, one such medication – omalizumab (or Xolair) – looks likely to become the first “anti-IgE” biologic drug contender to treat multiple food allergies.
Researchers from the Consortium of Food Allergy Research are studying omalizumab in two ways for child and adult patients. The first is as a standalone treatment to protect against reacting to accidental exposures in those with allergies to peanut plus two or more other foods: milk, egg, wheat, cashew, hazelnut or walnut.
The second method is as an add-on treatment for oral immunotherapy (OIT) to reduce adverse reactions and improve safety.
“If this drug works, it’s very likely to work for exposures to at least small amounts of any foods, where people could eat out without having to worry,” says Dr. Robert Wood. He’s the trial’s principal investigator and director of pediatric allergy and immunology at Johns Hopkins Medicine in Baltimore.
It’s quite possible omalizumab could help people safely eat more than small amounts of their allergens – perhaps even introducing these foods into their diets.
Stage 1: Xolair and Food Introduction
The first 60 participants have completed stage 1 of the double-blind, placebo-controlled study. At this stage, neither researchers nor patients know who is receiving the injectable medication and who is getting the sham shot.
The initial patients then moved to an “open-label extension” of the trial. Everyone, including those who had received the placebo injections, got a series of omalizumab injections. After six months of shots every two to four weeks, these patients underwent food challenges. Depending on how much they could consume of the allergens without reacting, patients could either immediately start introducing those foods into their diet, or start multi-allergen OIT.
“What we can say, even though the results are not fully analyzed, is that most of the participants were able to successfully introduce the foods they were allergic to into their diet,” Wood says.

Those who were able to eat a lot of the food at their food challenge without reacting are given a minimum and a maximum amount of the allergenic foods to eat daily. This is to maintain their desensitization. Those who reacted to smaller amounts of the food are offered OIT, since it starts at a lower dose of the food protein.
Stage 1 of the trial is still enrolling, with a goal of getting to 225 patients. “If things look good, this treatment could move out to the public in 2024 or possibly 2025,” Wood says.
Omalizumab is a monoclonal, or lab-made, antibody. It’s currently approved in the U.S. to treat moderate to severe asthma, nasal polyps and chronic hives. The drug, developed by Genentech and Novartis Pharmaceuticals, works by binding to IgE antibodies circulating in the blood. This prevents the IgE from binding to receptors on the surface of mast cells and basophils. Those immune system cells are involved in setting off allergic reactions and anaphylaxis.
Promise of Anti-IgE Medications
In 2018, the U.S. Food and Drug Administration granted omalizumab breakthrough therapy designation for its potential as a food allergy treatment. Wood and his colleagues launched the OUtMATCH study the following year.
Omalizumab, and anti-IgE medications like it, have long been eyed as a food allergy treatment. The first study to look at treating peanut allergy with monoclonal antibodies was published in 2003.
Back then, researchers gave 84 peanut-allergic patients either an injection of an anti-IgE drug similar to omalizumab, called TNX-901, or a placebo. They found that after a single dose of TNX-901, participants who had initially reacted to the equivalent of half to one peanut could consume almost nine peanuts before starting to react. TNX-901, however, was never developed for commercial use by the drug makers.
Even so, anti-IgE biologic drug research continued. As well as studying biologics as standalone treatments (called monotherapy) for food allergy, researchers also wanted to know if combining a biologic with OIT could cut down adverse side effects.
During OIT, allergic individuals eat gradually increasing amounts of their allergen over several months. The goal is to increase protection in case an allergen is accidentally consumed. While OIT has a strong success rate, many patients experience adverse effects. Common symptoms are mouth and throat itching, stomach pain or vomiting. A minority of patients experience anaphylaxis.
“We and many others had been pushing to move this forward,” says Wood. “One idea was using Xolair as a drug to treat food allergy. The second idea that has been studied is to use Xolair along with OIT as a way to make OIT safer.”
“The two approaches are going to look quite different, with one being a longer-term use of Xolair to increase the threshold of reactivity. While the other is a relatively short-term use of Xolair to get the dosing escalation done.”
Indeed, some allergists already prescribe omalizumab “off-label” in conjunction with OIT. Others will wait for FDA approval of such a protocol. Wood says FDA approval is also needed for insurance coverage.
Xolair Trial: Solo and Combo Therapies
The OUtMATCH trial was about 80 percent enrolled, as of October 2022. At the start of the study, all participants do oral challenges to confirm their food allergies.
From there, one group receives injections of omalizumab every two to four weeks, while the other group receives placebo shots. After four months, a second round of food challenges determines how much of each allergen patients can tolerate.
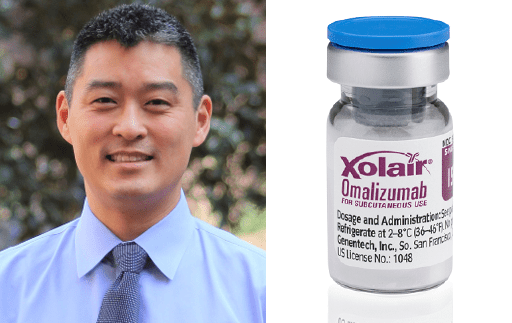
“We do think people can become protected to large amounts of food pretty quickly – 20-plus peanuts. That is what we are hoping to see,” says Dr. Edwin Kim, a study investigator and an associate professor of allergy and immunology at the University of North Carolina at Chapel Hill.
Additional stages are underway. Stage 2 looks at using Xolair with OIT. All Stage 2 participants receive omalizumab injections for the first eight weeks of treatment, then start either multi-allergen OIT or placebo OIT.
Then as oral immunotherapy begins, they receive the shots for the first eight weeks of treatment. After that, half the participants continue with multi-allergen OIT while receiving placebo shots. The other group continues with placebo OIT, but receives real Xolair injections. All participants then go onto maintenance therapy in their respective groups to complete one year of treatment.
Stage 3 will be a real-world follow up of patients to see how they fare over the long-term having introduced the foods into their diet.
“We are all very excited about this. Scientifically, it’s supposed to work. Hopefully we are correct, and it does work,” Kim says.
Age of Food Allergy Therapies Coming?
If Xolair is approved as a standalone treatment, the label would say the medication is for the prevention of reactions to small, accidental exposures to food, Wood says. Patients would still be advised to avoid their allergen. (Although they could potentially do a food challenge to see if they could tolerate more, he adds).
The dosing amounts and intervals in the trial are the same as the dosing of omalizumab when it’s used to treat other conditions. In patients 12 and older, omalizumab can be self-injected at home after several in-office injections. Researchers say they expect food allergy patients would be able to do the same.
If injections are stopped, Xolair’s effects will gradually wear off over several months. While omalizumab is usually considered very safe, it can have a range of side effects. These include rare but severe allergic reactions. The medication carries a “black box” warning about potentially life-threatening anaphylaxis.
Even with those caveats, Kim predicts the medication as a monotherapy would be a welcome option for many food allergy families, including those who choose not to pursue OIT.
OIT can be challenging for some families to manage. Parents’ work schedules and intense after-school sports schedules may make daily dosing and rest periods difficult. Many allergists aren’t set up to offer OIT, so accessibility is an issue in some areas.
“An Olympic-level swimmer who is training constantly maybe can’t do an OIT, but they can do a once a month shot,” Kim says. Omalizumab might provide added protection for teenager about to leave home for college. Or, an adult might choose the shots to feel safer when dining out and traveling.
To date, there is only one FDA-approved food allergy therapy – Palforzia, the oral immunotherapy for peanut allergy. While some allergists offer OIT for other foods, patients with many food allergies find it time-consuming to become desensitized to all of them.
“One of the most exciting things about a drug to treat food allergy as opposed to OIT is that a drug like Xolair would not be food-specific,” Wood says. “If someone had food allergies other than peanuts, or peanut plus eight other food allergies, instead of having to wait for an OIT product to be available, this would be a way to cover everyone’s food allergies equally.”
Kim says not to overlook that omalizumab as an adjunct to OIT is also exciting. If the medication can prevent adverse reactions during OIT, it could improve dropout rates during the dose escalation period. Or, it could help those worried about reactions to feel safer in trying it.
Kim envisions that one day soon food allergy families will have choices about what treatment route is best for them. “This is about creating options for people. Until we have that one-shot cure, it’s going to be about personalized medicine. Food allergies affect people in different ways,” he says.
Related Reading:
Allergists See Palforzia as Start of Era of Food Allergy Therapies
OIT Study See Maturing of Immune System Over Time
New Peanut Allergy Test Reveals if Trace Amounts Risky or Not