It’s the most dreaded phrase among patients of all kinds: “I don’t know.” When it comes to our health, we find comfort in answers and seek definitive causes with proven treatments. But sometimes, uncertainty can be a good thing. It’s a sign that we’re asking questions, exploring every angle, and never taking one solution as an absolute truth.
Such is the case with non-celiac gluten sensitivity. Virtually unrecognized a decade ago, gluten sensitivity is now a baffling puzzle that has prompted nearly 200 studies in the past two years alone. Today, we have more questions than ever, but that’s proof of our increasing research and knowledge, not the lack of it.
While it can be frustrating to have so many unknowns, it’s important to note that we’re not alone. Doctors and researchers are grappling with these questions, and they have a steadfast commitment to answering them. As Dr. David Sanders, chairman of the health advisory committee for Coeliac UK, reminded us recently: “We are still on a learning curve ourselves about this condition and its natural history, and patients need to understand that.”
One of the biggest questions to emerge recently – and an item of hot debate at the International Celiac Disease Symposium in late 2013 – is whether the explosive prevalence of gluten sensitivity is truly due to gluten, or whether other factors and food culprits could be part of the cause.
A link between gluten sensitivity and irritable bowel syndrome (IBS) has long been suspected, and new studies continue to reinforce the association. Recent research reveals that gluten or wheat sensitivity occurs in 28 to 30 percent of people with IBS, a prevalence rate that is much higher than in the general population.
What this tells us is that some people with IBS may benefit by removing gluten from their diets, and it may help to explain why gluten sensitivity appears to be more widespread than celiac disease. But at the same time, researchers emphasize that a gluten-free diet isn’t the solution for all people with IBS, and there are other factors to uncover.
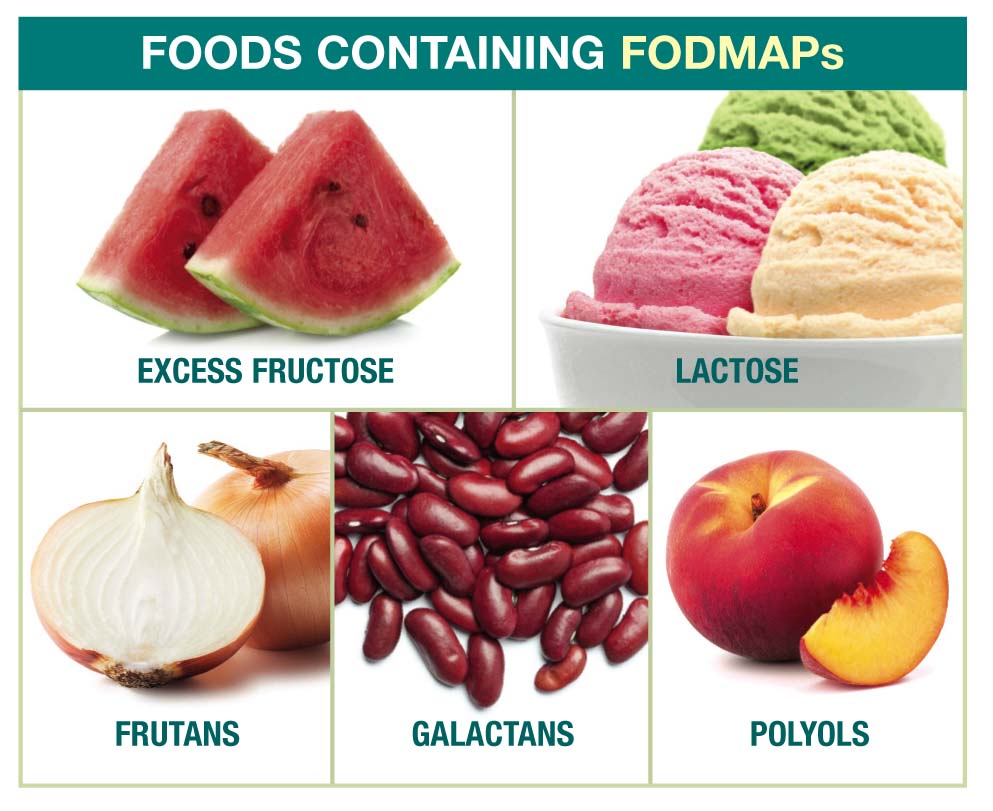
Another key area of research interest is FODMAPs, or Fermentable Oligosaccharides, Disaccharides, Monosaccharides and Polyols. FODMAPs include a variety of foods like onions, broccoli, beans, apples and milk that can be difficult for some people to digest.
Dietitian Susan Shepherd developed the low FODMAP diet in 1999 as a treatment for IBS, and over the last several years it has gained significant attention among both patients and researchers for effectiveness.
What’s particularly notable is that wheat, barley and rye are also on the list of FODMAPs, so there’s a crossover between the low FODMAP diet and the gluten-free diet. Researchers are curious whether the benefits of the gluten-free diet among people with gluten sensitivity may actually be a result of reducing FODMAP intake.
A study published in the journal Gastroenterology in June 2013 found that, in some people with gluten sensitivity and IBS, reducing the intake of FODMAPs alleviated symptoms better than the gluten-free diet.
However, other studies found that people with IBS and gluten sensitivity reported improved symptoms on a gluten-free diet, and the benefits remained even when high FODMAP foods like beans were reintroduced.
So what does this mean? Are FODMAPs the problem, or is it just gluten? Is IBS a part of the gluten-related disorders spectrum, or does it fall somewhere on its own separate branch?
It’s not necessarily one or the other. What these studies do reinforce is that we have a lot left to learn, and choosing absolutes will only limit our progress.
In the past, we have made the mistake of discounting a person’s symptoms simply because they didn’t fit the mold. But now, there’s a movement toward “personalized medicine,” which embraces the whole, individual person and considers everything from genetics to diet to symptoms in developing a specialized treatment.
Personalized medicine understands that what works for one person may not work for another, which is just what these studies on IBS and FODMAPs demonstrate. It’s the same reason we at NFCA always recommend that you make food and nutrition choices based on your individual health needs.
As we move along this learning curve, I guarantee that researchers will find new connections, surprising contradictions and even more questions about gluten-related disorders. Our role as patients will be to keep an open mind and embrace the shifting landscape.
Alice Bast is CEO of Beyond Celiac, the national organization working on behalf of the celiac patient community. Visit BeyondCeliac.org to learn more.