The American Academy of Allergy Asthma and Immunology has released a list of tests and procedures that are overused in the diagnosis and treatment of allergies. As research rapidly progressing in the field of allergy and immunology, best practices can become outdated, and not all physicians or patients are aware. Here are some of the key recommendations released by the AAAAI in the spring of 2014:
1. Don’t rely on antihistamines as a first-line treatment in severe allergic reactions.
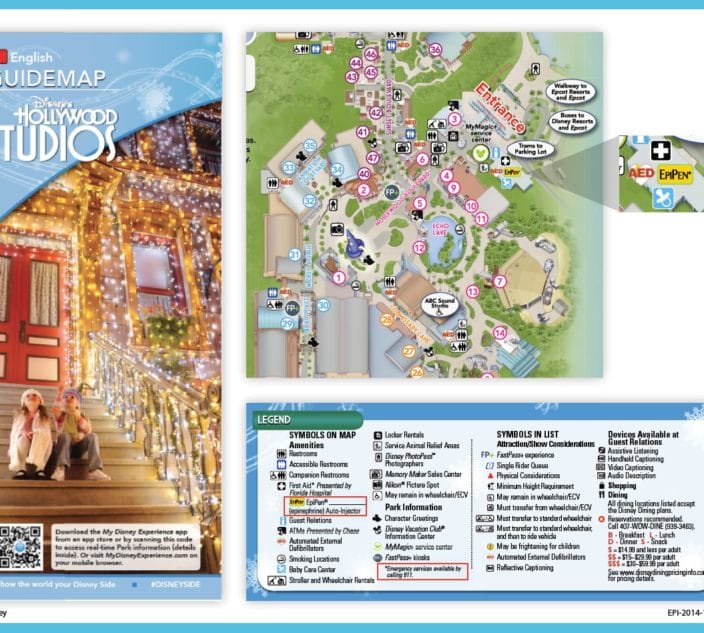
Readers of Allergic Living will know that there is only one first-line treatment for anaphylaxis: injection of epinephrine. Antihistamines can be used to reduce symptoms like hives and itching, but never to treat anaphylaxis. As the AAAAI notes: “Overuse of antihistamines, which do not treat cardiovascular or respiratory manifestations of anaphylaxis, can delay the effective first -line treatment with epinephrine.”
2. Don’t perform food IgE testing without a history consistent with potential IgE-mediated food allergy.
Performing such blood tests for foods that haven’t caused any reactions in the past can result in lowered quality of life due to unnecessary restriction of the diet – and increased health-care costs. These tests can produce false positives or clinically irrelevant results. IgE testing “must be driven by a history of signs or symptoms consistent with an IgE-mediated reaction after eating a particular food,” the report notes. And it should be limited to the suspect food or foods in question.
3. Don’t routinely order low- or iso-osmolar radiocontrast media or pre-treat with corticosteroids and antihistamines for patients with a history of seafood allergy, who require radiocontrast media.
In the past it was thought that people with shellfish allergy were more likely to react to radiocontrast material used for X-rays or other scans. However, “there is no cause and effect connection with seafood allergy,” notes the report.
Flu Vaccine and Penicillin
4. Don’t routinely avoid influenza vaccination in egg-allergic patients.
Certain vaccines, like those for measles, mumps, rabies, influenza and yellow fever, may contain egg protein. The report notes that for measles, mumps and rabies vaccines, the amount of egg protein is at most negligible, so no special precautions are needed for egg-allergic patients.
For the flu shot, egg-allergic patients should be given either the new egg-free influenza vaccine or should receive egg-based influenza vaccine with a 30-minute post-vaccine observation period. The report says 27 studies have collected data on 4,172 patients with egg allergy who received 4,729 doses of egg-based flu vaccine. There were no cases of anaphylaxis. “Studies in egg-allergic patients receiving egg-based inactivated influenza vaccine have not reported reactions,” it notes. However, for the yellow fever vaccination, it’s recommended to skin-test first, and observe for 30 minutes after the shot.
5. Don’t overuse non-beta lactam antibiotics in patients with a history of penicillin allergy, without an appropriate evaluation.
About 10 percent of the population reports a penicillin allergy, and it’s estimated that 90 percent or more of these people are not actually allergic to penicillin.
“The main reason for this observation is that penicillin allergy is often misdiagnosed and when present wanes over time in most (but not all) individuals,” notes the report. These patients are also more likely to have increased medical costs, longer hospital stays and to develop complications like antibiotic-resistant infections.