Some must say goodbye to crisp apples. For others, it’s adieu to juicy peaches, tomatoes and melons, carrots or celery – and more. The condition they have is oral allergy syndrome or OAS, which is an allergy to a variety of raw fruits and vegetables. Read expert insights into the condition, and see our chart of foods that can cross-react. [Updated May 2022.]
Nothing gives me that sense of reckless abandon like running barefoot through green grass and feeling the heat of the sun on my skin. And who doesn’t look forward to the cornucopia of fresh produce that summer weather brings? That first juicy bite of a ripe peach; the satisfying crunch of a crisp carrot; the requisite snap of a newly picked snap pea. Is there anything to rival these summertime indulgences?
Alas, however, I must take vicarious satisfaction in watching others enjoy summer’s rich bounty. For me, a few tempting bites of certain fruits or vegetables will soon be followed with rather unpleasant sensations – a tingly throat, and an itchy mouth and tongue. The bane of oral allergy syndrome (OAS) strikes again!
OAS, also known as pollen-food syndrome, is a form of food allergy linked to certain raw fruits and vegetables, as well as nuts, and even seeds and spices. This syndrome actually emerges because of allergies to the pollens of certain trees or grass or ragweed. For those with OAS, the immune system “sees” the proteins of some fruits and vegetables as being much like the pollen protein – and a cross-reaction ensues.
“It’s called a Class 2 food allergy,” says Dr. Anna Nowak-Wegrzyn, director of the pediatric allergy program at Hassenfeld Children’s Hospital at NYU Langone. “You first become allergic to a pollen via inhalation, and then start reacting to foods that share similar proteins. So this food allergy is secondary to the pollen allergy.”
Birch tree pollen is a big offender. Nowak-Wegrzyn, who has researched the syndrome, says that anywhere from 30 to 70 percent of people with birch pollen allergy have OAS. “It’s a very common condition,” she says.
Oral Allergy Signs
So how can you tell if you’ve got OAS? How do you know which ripe produce to avoid, which will be safe for the picking, and whether you’re susceptible to a more serious reaction? Let’s delve into the answers.
Symptoms of the syndrome can include itchy, tingly, scratchy or swollen mouth, lips, tongue, throat, palate or ears; watery, itchy eyes, runny nose and sneezing. The symptoms typically last only minutes to an hour. In my case, I will get the itch and tingle throughout my mouth – lips, tongue and throat. Thankfully, it usually dissipates in 20 minutes.
“There is a contact reaction in the mouth and throat of itching or swelling. It’s pretty immediate, but usually quite mild,” says Nowak-Wegrzyn.
Cooking Benefits
Unlike other food allergies, with oral allergy, she says once an offending fruit or vegetable hits the stomach, “digestive enzymes break down the proteins and symptoms resolve.”
If you’re like me and sometimes crave a fruit fix, opt for cooked versions like apple sauce, peach cobbler or cherry pie. Unlike allergies where antibodies are created to specific foods, with OAS the thorough cooking will break down the proteins enough to keep some produce within reach.
Even though I have relatively mild oral allergy symptoms to raw foods, this doesn’t mean they aren’t bothersome. The one time I gobbled down an entire peach, my lips puffed up like lip fillers in overdrive. While some might envy such a look, it was wickedly uncomfortable, so I’ve not caved to temptation like that again.
What Foods Cross-React?
I never understood why some of the fruits that cross-react with birch pollen, like my beloved peaches, posed a problem. Yet others, like pears and kiwis, I could eat to my heart’s delight. Dr. Antony Ham Pong, a Canadian allergist and researcher, has the explanation. “When you have a birch allergy, fruits have similar allergens, but not exactly the same. That’s why sometimes you may react to some foods and not to others,” he says.
Foods like apples, peaches, carrots, celery and hazelnuts have a higher incidence of cross-reaction with birch protein. For those with grass allergies, fresh melons and tomatoes commonly set off OAS reactions, while melons, bananas and cucumbers can bring on oral symptoms in the ragweed-allergic.
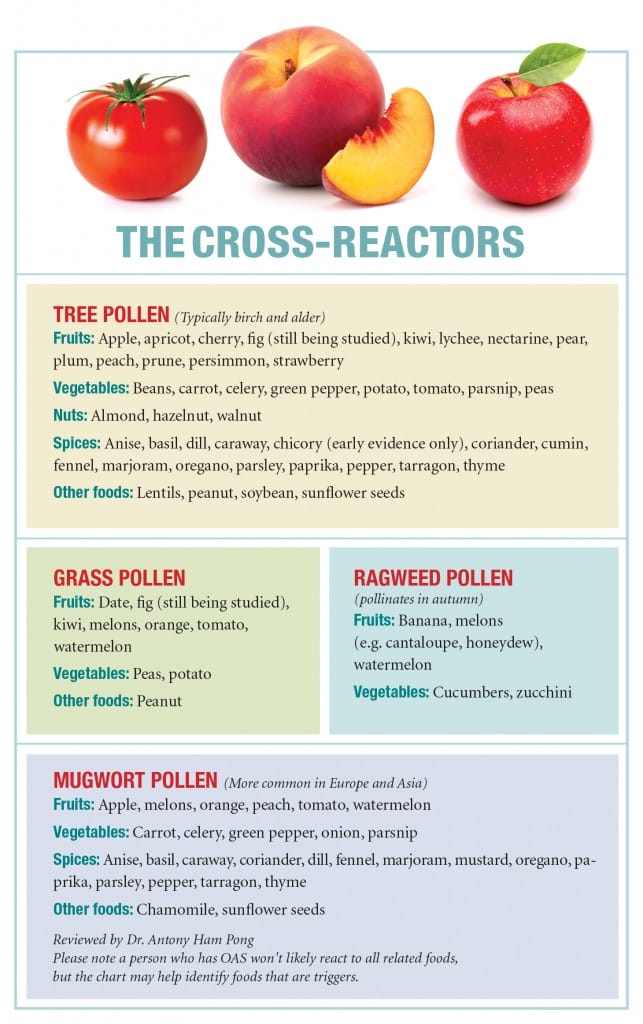
Oral Allergy Cross-Reactors Chart
While the list of what foods and spices cross-react is especially long for those sensitized to birch pollen, the experts say that you only need to avoid the foods that trigger a reaction. However, Ham Pong says it’s important to be aware that over time, your OAS may progress so that you have more reactions to more foods.
Whether you have an OAS reaction can be affected by the season, the type of food, its ripeness and even what variety it is. For instance, Granny Smith and Golden Delicious apples may be more likely to set off an oral allergy, while Fuji, Braeburn and Santana are least likely. An unripened fruit often leads to a milder allergic reaction than one that’s very ripe.
This can make OAS tricky to diagnose. “It is far more common than we realize,” asserts Ham Pong. “Patients often don’t bring it up to their doctors because it doesn’t make sense. They get a reaction from eating an apple but not from apple juice so they think, ‘it can’t be an allergy.’ They think they are crazy! Many people who have OAS ignore the symptoms because they are mild and inconsistent.”
Testing for OAS Culprits
Both Ham Pong and Nowak-Wegrzyn suggest speaking to an allergist if you experience symptoms, since you likely need to be tested for IgE antibodies to pollens, as well as to the foods causing you trouble. (The experts say food testing should be performed with fresh raw foods as commercial extracts can result in false negatives.)
If you show positive results for certain foods, Nowak-Wegrzyn says you can take it a step further with component blood testing, a molecular diagnosis that measures specific IgE antibodies against pollen and implicated foods. This way, you’ll get a more reliable read on the severity of the allergy.
“If you only make antibodies against cross-reactive components in the food, it is extremely unlikely you would get a systemic reaction or anaphylaxis,” she says. “If you make antibodies against components that are specific to the food and not the pollen, then it’s more likely. It’s important to know, as it makes a big difference in how to manage the allergy.”
When Oral Allergy is Severe
While most of us only get oral reactions, Ham Pong says some people with pollen-food syndrome experience severe symptoms, such as vomiting, cramps and diarrhea. As well, “about 2 percent of those with OAS can have an anaphylactic reaction,” he notes. They get additional symptoms such as swelling of the throat, trouble breathing and hives. Foods such as nuts, celery, peaches and apples are most commonly associated with the serious reactions.
The amount you eat of an allergenic food, and whether you’re exercising or drinking alcohol can influence the level of response, too. Ham Pong gives an example of some severe cases he has seen, related to a concession stand in a popular park.
“After running, people would get a glass of freshly squeezed carrot juice from this stand. They would then have an anaphylactic reaction.” The combination of exercise and quickly consuming a large volume of raw juice sets off the more severe reaction, since the body does not have time to give warnings in the form of milder symptoms, and the digestive enzymes cannot counteract the allergic proteins fast enough.
Plus, the incidences took place at the height of pollen season when, Ham Pong says, “OAS can worsen because of exposure in mouth, nose and lungs, and result in a more severe reaction.”
Still, he doesn’t prescribe epinephrine auto-injectors to all his OAS patients, though some allergists do. Instead, he works with patients to assess the risk and the need for the device. “If you’ve ever had a serious reaction, then yes for sure. If you’ve only had mild reactions, I tell patients they can continue to eat the food cooked. If they have a reaction with cooked, then stop,” he says.
Nowak-Wegrzyn cautions, though, that allergies can come to involve more foods. “If oral symptoms start getting progressively worse, then they should be re-evaluated,” she says. “It’s a red flag that this is no longer just pollen cross-activity.”
Life with Less Raw Fruit
For the majority of us with milder OAS, it can involve some trial and error to figure out which on a long list of related foods you’ll react to. For those who simply have the pollen cross-reaction, Nowak Wegrzyn says the strict rule of complete allergen avoidance, which is vital for the safe management of classic food allergy, is slightly more relaxed. That means you may be able to have a few bites of an apple or peach, but just need to pay close attention to whether any symptoms arise.
If you do have even a mild reaction and have tested positive for a related pollen allergy, Ham Pong says it is time to stop eating that raw fruit or vegetable altogether. “It’s like you’re crawling along a branch, and it begins to creak. You need to make a decision; do you keep going or do you back off? It’s a warning sign; you might be OK, but you might not.”
Instead, you can stick to berries, citrus fruits or grapes, which are not usually cross-reactive with pollen. Peeling fruit can help as the peel has more allergens, as can cooking or microwaving the food to break down the offending proteins. Taking daily doses of antihistamines is not recommended for pollen-food syndrome since the pills may prevent the symptoms that warn you to stop eating a food. Plus, they will not stop anaphylaxis.
Ultimately, OAS is still a form of food allergy, so you need to respect that. If you have an OAS reaction to a food, it’s best to avoid it. “It’s really just common sense,” says Nowak-Wegrzyn.
Related Reading:
All About Oral Allergy Syndrome
Believe Me, I Do Have Oral Allergy Syndrome
Oral Allergy: Plants, Foods That Cross-React