Updated Summer of 2021 – Researchers are enrolling participants in a study to determine whether people with severe allergies or a mast cell disorder are at higher risk of allergic reactions to the COVID-19 mRNA vaccines than those without allergies. [Editor’s Note May 18, 2022: Read about the final findings of the study here.]
The clinical trial is seeking adults ages 12 to 69, and the study will involve up to 29 centers across the United States.
“The public understandably has been concerned about reports of rare, severe allergic reactions to the Moderna and Pfizer-BioNTech COVID-19 vaccines,” said Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases (NIAID), when the study was announced in April 2021. (NIAID is part of the National Institutes of Health, the trial sponsor.)
“The information gathered during this trial will help doctors advise people who are highly allergic or have a mast cell disorder about the risks and benefits of receiving these two vaccines. However, for most people, the benefits of COVID-19 vaccination far outweigh the risks,” said Fauci.
Since the Pfizer-BioNTech and Moderna COVID-19 vaccines rollout began in December 2020, millions of Americans – including those with severe allergies to foods, drugs and insect venom – have received the vaccines without any problems.
But reports of rare cases of anaphylaxis have led to questions about whether people with a history of allergies or mast cell disorders are more likely to have allergic reaction to the vaccines, and if so, why. The majority of anaphylactic reactions have been reported in women and in people with a history of allergies to a wide range of triggers, including foods, drugs, injectable medications or contrast dye.
Most Subjects Will Be Women
The multi-center trial is enrolling several hundred people adults with a history of severe allergic reactions or mast cell disorder, a condition in which people experience episodes of anaphylaxis without a known allergy trigger. There is also a large control group of people without allergies. Two-thirds of participants will be women.
Participants will be randomly assigned to receive either the Pfizer vaccine, the Moderna vaccine, or a placebo during their first visit. (The first part of the study is “blinded,” so that neither study subjects nor researchers know who got the actual vaccine with the first shot.)
Everyone gets an actual vaccine shot on the second visit, and three days after receiving that, participants will learn which dose they initially received.
During a visit for a shot, the participants will be observed for 90 minutes by allergists who are able to treat any reactions. Blood, urine and nasal swabs will be taken before each dose is given, and blood and urine will be taken after each shot.
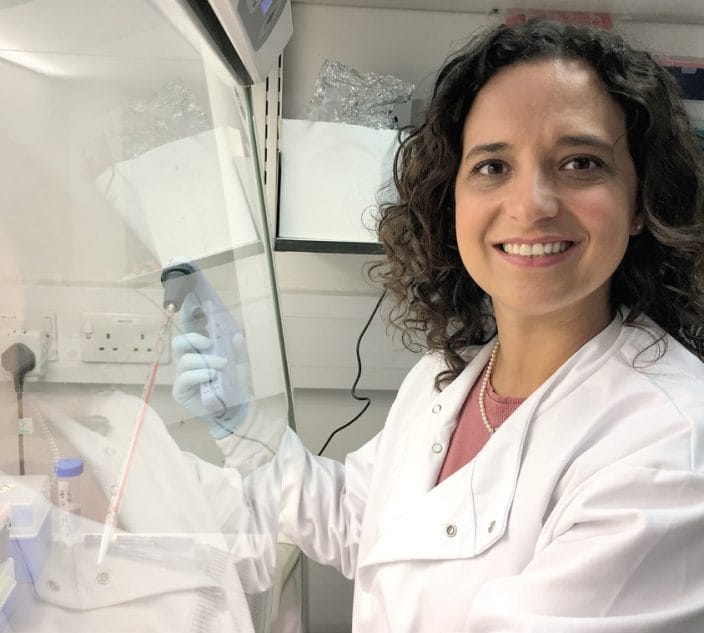
If there are any reactions, researchers will analyze the samples and run genetic tests to try to determine what type of reaction occurred, says Dr. James R. Baker, co-chair of the study and director of the Mary H. Weiser Food Allergy Center at the University of Michigan.
Participants in the placebo group for the first shot will have their second dose scheduled at the appropriate interval, which is three weeks for the Pfizer vaccine and four weeks for Moderna.
“Everyone in this study will receive either the Pfizer or the Moderna vaccines,” Baker says. Results of the study are expected in late summer.
Allergies Vs. Mast Cells Activation
A U.S. Centers for Disease Control and Prevention (CDC) study puts the anaphylaxis rate at 2 to 5 people per one million vaccinations with the Pfizer-BioNTech or Moderna mRNA vaccines.
The rate of reactions to the mRNA vaccines seems a bit higher than the 1.31 in one million previously reported for other vaccines, such as the flu shot. “The rate may be slightly higher, but it’s certainly not orders of magnitude higher,” Baker notes.
With the mRNA vaccines, a study of 65,000 people vaccinated at Massachusetts General Hospital found about 2 percent reported milder symptoms that might indicate an allergic reaction.
Yet the causes of the reactions are unknown. Speculation about triggers has included an IgE-mediated allergy to polyethylene glycol (PEG), an ingredient in the mRNA vaccines. However experts, including Baker, say that is a very rare allergy.
Another explanation could be activation of mast cells through another, non-IgE mediated immune system process, which can mimic an allergic reaction.
Recently, researchers have suggested that some people’s mast cell receptors might be prone to over-responding to the small amounts of mRNA in the vaccines. Reactions involving the direct activation of mast cells tend to be less severe than a typical allergic reaction. “Immune reactions involving mast cell triggers tend to be less explosive than an IgE-mediated reaction,” Baker says.
In the reports of anaphylaxis after the mRNA vaccines, most people have reported what are considered lower-level anaphylactic reactions, including “cutaneous” symptoms such as a face swelling, hives, itching and rash, but not more serious symptoms, nor anaphylactic shock.
In the new clinical trial, if some patients react to the vaccine, researchers will conduct whole genome screening to see if any particular genetic variants are associated with the reactions to the vaccines, and whether people with a history of allergies are more likely to have those variants.
How Can I Enroll in the Study?
Locations:
The NIH study includes sites in 20 states, including: Arizona, Arkansas, California, Colorado, Florida, Georgia, Illinois, Iowa, Maryland, Massachusetts, Michigan, Missouri, New York, North Carolina, Ohio, Pennsylvania, Tennessee, Texas, Virginia and Wisconsin. (See information on the specific centers enrolling below.)
Eligibility:
Allergy Group: Participants in the allergy group must have a history within the last five years of a severe reaction to foods, allergen immunotherapy, or insect venom; an immediate allergic reaction to two or more drugs; or a convincing clinical history, including a positive skin test, of a reaction to a drug or vaccine. The study will also include people diagnosed with a mast cell disorder. Learn more on eligibility here.
Non-Allergy Group: People in the non-allergy group must have no history of allergic disorders, including allergic asthma, rhinitis, eczema or chronic hives.
Exclusions:
Among those excluded are: people who have taken a biologic therapy within six months of the trial, anyone who has used oral steroids within 28 days, or anyone who has recently had the coronavirus.
Compensation:
A study website launched in June says volunteers will be compensated for their time.
Centers Now Enrolling:
University of Arizona Health Sciences, Department of Medicine, Division of Pulmonary, Allergy, Critical Care and Sleep Medicine, Tuscon, AZ
Principal Investigator: Tara F. Carr, MD
Contact Chelsey Large: 520-626-5590; [email protected]
Arkansas Children’s, University of Arkansas for Medical Sciences, Little Rock, AR
Principal Investigator: Stacie M. Jones, MD
Contact Mary Kemp: 501-398-8622; [email protected] or Vallon Williams: 501-398-8622; [email protected]
University of California, Los Angeles Medical Center, Los Angeles, CA
Principal Investigator: Maria Garcia-Lloret, MD
Contact Alexis Stephens: 310-210-8771; [email protected]
Stanford University, Sean N. Parker Center for Allergy & Asthma Research, Stanford CA
Principal Investigator: Sayantani (Tina) Sindher, MD
Contact Laurie Kost: 650-521-7237; [email protected]
National Jewish Health, Denver, CO
Principal Investigator: Donald YM Leung, MD, PhD
Contact Ashley Kohlhepp, RN: 303-270-2145; [email protected]
University Health, University of Miami Health System, Miami, FL
Principal Investigator: Gary Kleiner, MD, PhD
Contact Alejandra Weisman: 305-243-1425; [email protected]
University of South Florida Asthma Allergy and Immunology Research Unit, Tampa, FL
Principal Investigator: Thomas Casale, MD
Contact Catherine Renee Smith, CMA: 813-631-4024 ext 207; [email protected]
Emory University School of Medicine, Emory Clinic Allergy and Immunology, Atlanta, GA
Principal Investigator: Merin Kalangara, MD
Contact John Varghese, MS: 404-727-2886; [email protected]
Sinus and Allergy Center of Northwestern University, Chicago, IL
Principal Investigator: Anju T. Peters, MD
Contact Amina Guo: 248-525-2060; [email protected]
NorthShore University Health System, Dermatology Clinical Trials Unit, Skokie, IL
Principal Investigator: Giselle Mosnaim, MD
Contact Site Public Contact: 847-663-8522; [email protected]
University of Iowa Health Care, Iowa City, IA
Principal Investigator: Mary Beth Fasano, MD, MSPH
Contact Amy Mundisev, RN,MSN: 319-356-1445; [email protected]
Johns Hopkins Bayview Medical Center, Baltimore, MD
Principal Investigator: Melanie Dispenza, MD, PhD
Contact: Jeanne Hoddinott, RN: 443-686-8154; [email protected]
Massachusetts General Hospital, Boston, MA
Principal Investigator: Kimberly Blumenthal, MD, MSc
Contact Site Public Contact: 617-726-3627; [email protected]
Brigham and Women’s Hospital, Boston, MA
Principal Investigator: Mariana Castells, MD, PhD
Contact Sahar Hamadi: 617-732-9850; [email protected]
University of Michigan Health, Ann Arbor, MI
Principal Investigator: James R. Baker Jr., MD
Contact Courtney Oliver: 906-273-2145; [email protected]
Henry Ford Hospital and Health System, Detroit, MI
Principal Investigator: Edward Zoratti, MD
Contact Shannon Murray: 313-805-5718; [email protected]
Saint Louis University Care Center for Specialized Medicine, Saint Louis, MO
Principal Investigator: Mark Dykewicz, MD
Contact Site Public Contact: 866-410-6333; [email protected]
Mount Sinai Hospital, Department of Medicine, Division of Clinical Immunology, New York, NY
Principal Investigator: Paula J. Busse, MD
Contact Shanti Mangar, MPA, CCRC: 646-320-5303; [email protected]
Columbia University Irving Medical Center, New York, NY
Principal Investigator: Magda Sobieszczyk, MD, MPH
Contact Ian Horton: 212-342-2958; [email protected]
Rochester Regional Health, Rochester, NY
Principal Investigator: Allison C. Ramsey, MD
Contact: Dawn Sheflin, RN: 585-922-9314; [email protected]
North Carolina Clinical & Translational Research Center (CTRC) at UNC at Chapel Hill, NC
Principal Investigator: David B. Peden, MD
Contact Martha Almond: 919-966-2879; [email protected]
Cleveland Clinic, Allergy & Clinical Immunology, Cleveland, OH
Principal Investigator: David M. Lang, MD
Contact JoAnne Baran-Smiley, BSN, RN: 216-444-5023; [email protected]
Penn State Health Allergy, Milton S. Hershey Medical Center, Hershey, PA
Principal Investigator: Timothy Craig, DO
Contact Kristina Richwine: 717-531-4513; [email protected]
Vanderbilt University Medical Center, Nashville, TN
Principal Investigator: Elizabeth J. Phillips, MD
Contact Amy Kerrigan, MSN, RN: 615-322-6928; [email protected]
University of Texas Southwestern Medical Center, Dallas, TX
Principal Investigator: David A. Khan, MD
Contact Erika Molina: 214-799-0751; [email protected]
Baylor College of Medicine Medical Center, Houston, TX
Principal Investigator: Sanjiv Sur, MD
Contact Sherilyn Pillack: 713-798-0135; [email protected]
University of Virginia Health System: Division of Allergy and Immunology, Charlottesville, VA
Principal Investigator: Michael R. Nelson, MD, PhD
Contact Deborah Murphy, RN: 434-982-3510; [email protected]
Virginia Commonwealth University, Division of Rheumatology, Allergy & Immunology, Richmond, VA
Principal Investigator: Lawrence B. Schwartz, MD, PhD
Contacts Esperanza Gilbert: 804-828-4700; [email protected] or Esoterica Berry: (same phone); [email protected]
University of Wisconsin Asthma Allergy Pulmonary Research, Madison, WI
Principal Investigator: Mark H. Moss, MD
Contact Mary Jo Jackson, BSN, RN: 608-265-3556; [email protected]
For more information on the study and locations: Visit the COVIDvaccine-allergy.org website or ClinicalTrials.gov, where the study identification number is NCT04761822.
Related Reading:
Few Severe Reactions to COVID-19 Vaccines, But Women Most Affected
FAQ on: Allergy Concerns and the mRNA COVID-19 Vaccine