The incidence of emergency treatment of anaphylaxis, the severe form of food-allergic reaction, climbed a remarkable 377 percent in the United States between 2007 and 2016, according to an extensive analysis of private health insurance claims.
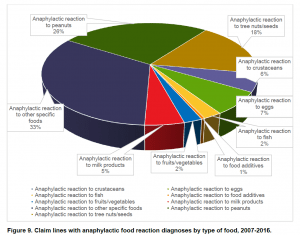
Among the foods triggering severe reactions, peanut was the single allergen most frequently seen in anaphylaxis (26 percent of cases), while tree nuts and seeds came in second (18 percent of cases). The tree nuts and seed category saw the biggest increase in severe reactions – a growth of 603 percent over the decade, while peanut anaphylaxis rose by 445 percent in that period.
The analysis, conducted by the nonprofit FAIR Health, finds the largest single anapylaxis trigger was “other specific foods,” a catchall category that includes: Top 8 triggers soy and wheat (which are not allotted separate insurance codes), several less common food triggers and cases in which the food trigger was simply not known.
While food allergy is often viewed as a childhood condition, the FAIR Health report reveals that those over the age of 18 accounted for more than one-third of diagnosis insurance claims.
Commenting on the 377 percent surge in anaphylaxis, Dr. James Baker, CEO* of the nonprofit Food Allergy Research & Education (FARE), told Allergic Living: “We think this shows definitive evidence for a dramatic rise in the number of severe, systemic and life-threatening food-allergic reactions that children and adults across the country experience every day.” FARE gave funding to this study of recent food allergy trends and costs in the United States.
Robin Gelburd, FAIR Health’s president, said she hopes this data “provides useful information for researchers, policy makers and other healthcare stakeholders.” FAIR Health keeps a database of billions of private health claims, which it analyzes in support of transparency of healthcare costs and trends.
Financial Burden with Milk Allergy
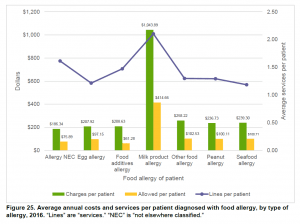
The financial burden to both families living with milk allergy and to the overall costs to the healthcare system becomes apparent in this analysis. A family who has a child with a milk allergy has the highest per patient cost of any food allergy, spending an average of $1,043 per year in health services and other costs.
To compare, someone with a peanut allergy spends an average of $236 per year on allergy-related costs. Those managing a milk allergy often have to buy specialized formula for a child, which is costly.
As for healthcare costs, over the 2007 to 2016 period, the charges for laboratory services associated with the diagnosis of anaphylactic reactions increased an astonishing 5,390 percent although the report doesn’t offer an analysis to indicate why such a steep rise.
Other Findings of FAIR Health:
• Only 2 percent of those who sought emergency care for anaphylaxis went to an emergency room. Although allergists recommend calling 911 in anaphylaxis, which is considered a medical emergency, health claims showed 70 percent of the care for severe reactions had taken place in physicians’ offices.
• The report gives further evidence of a rise in adult-onset allergies, with 34 percent of health claims for food allergy diagnosis being made for patients over the age of 18. “The increased prevalence in adults may reflect changes in the maturation of these individuals’ immune systems and environmental factors,” says Baker, who’s also FARE’s chief medical officer.
• More boys than girls develop food allergies, but the gender prevalence switches in adulthood: more women develop food allergies than men.
• The report identifies an emerging allergen category among women: food additives, which can include preservatives, sweeteners, colors, emulsifiers and stabilizers.
• There was growth in food allergy diagnoses in both urban and rural areas over the 10-year period, but the fastest growth was in rural settings – an increase of 110 percent compared to 70 percent in large cities.
“What the data shows is that food allergy rates are increasing nationwide, in rural and urban areas alike,” said Baker. “We need increased awareness of food allergy in all communities, so that everyone affected by this epidemic can benefit from appropriate medical care and a respectful, inclusive environment.”
The report analyzed 24 billion health care claims records from more than 150 million privately insured patients.
*Dr. Baker is now the former CEO of FARE.
All graphs courtesy of FAIR Health from the report: Food Allergy in The United States: Recent Trends and Costs – An Analysis of Private Claims Data.