 Visits to the emergency room for anaphylaxis in children climbed 150 percent from 2010 to 2016, according to a Blue Cross Blue Shield Association (BCBSA) report released in March 2018.
Visits to the emergency room for anaphylaxis in children climbed 150 percent from 2010 to 2016, according to a Blue Cross Blue Shield Association (BCBSA) report released in March 2018.
As well, the number of children diagnosed as at-risk for anaphylaxis doubled in that time period.
The seven-year BCBSA analysis takes an in-depth look at anaphylaxis and allergies in general among 9.6 million American kids under the age of 18 who have Blue Cross Blue Shield medical coverage.
Allergic Living breaks down the numbers and key takeaways from the report:
– Children diagnosed as at risk for an anaphylactic reaction rose 104 percent, or 47 per 10,000 children as of 2016.
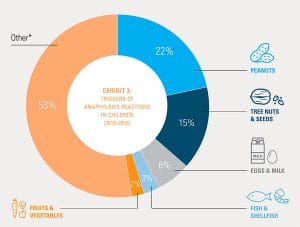
– Food accounted for 47 percent of children’s anaphylactic reactions in 2016. The specifics are: 22 percent of kids reacted to peanuts, 15 percent reacted to tree nuts and seeds, and 6 percent reacted to milk and eggs.
– However, 53 percent of anaphylactic reactions are attributed to unknown foods or unspecified triggers, which BCBSA says includes insect bites.
– Meanwhile, 3 percent reacted to fish and shellfish and 2 percent reacted to fruits and vegetables.
– There was a slight increase in children affected by all allergies. From rhinitis to food and atopic dermatitis – the rate rose from 17 percent in 2010 to 18 percent in 2016.
– The better news was evidence of a drop in allergy diagnosis as kids get older. The report found that 25 percent of infants up to age 2 are diagnosed with one or more allergies compared to 14 percent of teens, ages 14 to 18.
– Hay fever affected 9 percent of kids and eczema affected 5 percent.
– The average ER visit for anaphylaxis costs $1,419. Patients pay $373 out-of-pocket.
 Blue Cross Blue Shield Association
Blue Cross Blue Shield Association “Parents are recognizing symptoms, calling their pediatricians and coming to the ER a lot quicker,” Haywood said. “This report highlights the need for parents and guardians of at-risk children to be prepared for a reaction at any time.”
Similar trends have been identified in previous studies. A report based on private health claims from the non-profit FAIR Health found that the incidence of emergency treatment for anaphylaxis climbed a remarkable 377 percent in the U.S. between 2007 and 2016. Based on health claims from 150 million privately insured patients, that report also found that, among food triggers, peanut was the allergen most frequently identified in anaphylactic reactions (at 26 percent). However, “other foods” was the largest trigger category.
In another study published in 2017, Northwestern University pediatrician Dr. Ruchi Gupta found a 21 percent increase in peanut allergy in children over a six-year period as well as an 18 percent rise in tree nut allergies.
See the full BCBSA report here.





